Being stuck in negative emotions is a predominant symptom of depression. The effort to pull oneself out of this cycle of negativity seems an impossibility. When this state persists, other negative symptoms pile on to make this condition feel insurmountable. For some, but not all, relief is achieved through the combination of psychotherapy and medication. For others not helped by conventional treatment for depression, alternative less conventional methods are sought. One of these non-conventional modalities is ketamine assisted psychotherapy – the combination of ketamine (a mild, dissociative, psychedelic substance) and guided therapeutic assistance. For either approach, it is useful to understand the underlying factors/forces which feed depression regardless of the precipitating cause. Specifically, we are talking about how depression causes changes in the structures of the brain and how “medicine” and re-thinking our depression can help reverse these processes and produce lasting positive changes.
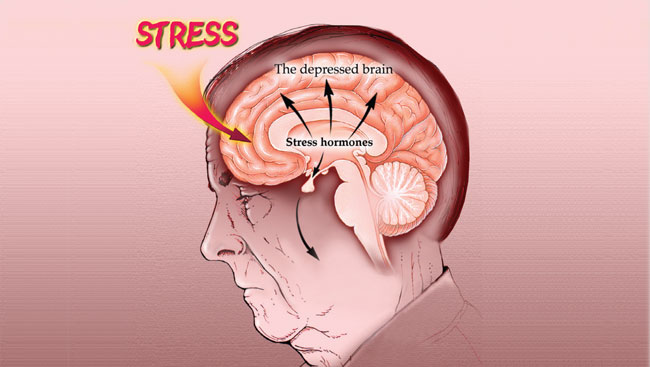
What Happens To The Brain When We Are Depressed:
*Research shows that clinical depression can in fact:
- Shrink the brain
- Cause brain inflammation
- Reduce oxygen levels in the brain
*Source: WebMD Article by, Keri Wiginton (Reviewed by Smitha Bhandari, MD., 7/28/2020)
The Brain Shrinks
Studies show that people with clinical depression tend to have shrinkage in certain regions of the brain. Even though researchers debate which regions of the brain appear to be most affected, data consistently shows an association between clinical depression and shrinkage in the following areas of the brain:
- Hippocampus, which plays an important role in learning and memory. The hippocampus also helps regulate emotions and stress hormones. As depression starts to affect the brain’s chemical balances, neurons in the hippocampus shrink, which can cause difficulty concentrating and memory loss. A shrunken hippocampus can also make completing familiar tasks difficult, which can lead to hopelessness, guilt, and anxiety.
- Prefrontal cortices control impulses, adapt to challenges, process and regulate emotions, think rationally, and plan. When these areas of the brain shrink, individuals can become impulsive and easily irritated, agitated, and upset. They might also experience brain fog - trouble thinking clearly, memory loss, and difficulty making decisions.
- Thalamus regulates sleep, alertness, and wakefulness. A shrunken thalamus has trouble maintaining a healthy sleep pattern, which often affects an individual’s appetite and wellbeing.
Generally, the amount of shrinkage that occurs depends on the severity and amount of time an individual experiences depression.
Brain Inflammation
Clinical depression can also inflame the brain. Experts aren’t 100% sure if inflammation causes depression or vice versa, but studies have shown a connection between the amount of time an individual has been depressed and the level of inflammation in the brain. Clinical depression seems to have a particular inflammatory effect on the amygdala. The amygdala is an almond-shaped gland that influences whether individuals feel pleasure or fear. The high levels of cortisol released during a depressive episode inflame the amygdala causing the gland to become hyperactive and enlarged. When this happens, individuals can experience disrupted sleep patterns, social anxiety, restlessness, guilt, panic, and self-blame.
Brain inflammation can also cause brain cell death. This can lead to further brain shrinkage and decreased neurotransmitter function. Brain inflammation can also make the brain less neuroplastic, or capable of changing. New brain cells stop growing. Older brain cells incur damage and die, causing the entire brain to age faster.
Brain inflammation also slows down firing between neurons. The overall operation of the brain slows down. Individuals’ thinking becomes slow and fuzzy. They feel fatigued and irritable. Their energy level declines, and they move slowly.
* Inflammatory immune cells called cytokines interfere with serotonin levels, affecting individuals’ ability to feel joy
Reduced Oxygen Levels
Clinical depression has also been linked to reduced oxygen in the body. This is a medical condition called hypoxia. When the brain doesn’t get the amount of oxygen it needs to function properly, brain cells can die. In fact, brain cells begin dying with 5 minutes of oxygen loss. At first, individuals might experience:
- Inattentiveness
- Poor judgment
- Temporary memory loss
- Trouble moving parts of the body
The longer individuals don’t have proper oxygen levels, the more severe the symptoms can become. Severe symptoms of hypoxia typically include:
- Coma
- Seizure
- Brain death
